The history of technological innovation, from the industrial revolution to the present day, has been one of extraordinary leaps in productivity. Processes are refined and honed; costs are driven out; new tools are developed to cut the time and effort required to make things. Technology is shaping our professional and personal lives at an unprecedented pace.
With the advent of AI and advanced robotics, driverless cars and quantum computing, it seems to many observers that technology is capable of virtually anything. As Arthur C. Clarke put it, “any sufficiently advanced technology is indistinguishable from magic”.
The ability of AI to analyze vast datasets, find patterns and highlight anomalies, for example, makes it easy to imagine the opportunities and challenges. In the lab, the advances have been even more extraordinary. In little over 100 years, we have gone from coining the term “gene” to routinely editing them or altering their expression. For the families of those living with a rare disease, drug research and development can seem comparatively slow – but recent advances could help accelerate the process.
Innovation and technology advances give rise to enormous potential for improving the lives of people living with rare diseases, but they face several significant challenges that can slow progress and limit impact. Economic incentives, for example, present a sizable obstacle. Since rare diseases impact very few patients, pharmaceutical companies and institutional investors often hesitate to look at the expensive R&D required to find lifesaving drugs, instead focusing on more mass-market candidates.
Although regulatory incentives help, the cost and time frames for rare disease drug development can still be prohibitive. Overcoming these barriers requires coordinated efforts, including data-sharing frameworks, institutional partnerships, patient involvement, and thoughtful regulation. Only by addressing these can those much-needed innovations translate into life-saving therapies. AI holds out the promise of transforming all of these issues, and it’s already making deep inroads into what once seemed intractable problems.
Data science
One of the most pressing issues for rare disease treatment innovation is data scarcity and fragmentation. Rare diseases, by definition, affect smaller populations, making it difficult to collect sufficient clinical data for accurate analysis. The data that does exist is often siloed across hospitals, research centers, or pharmaceutical companies, making comprehensive analysis and collaboration difficult. Without access to unified, high-quality datasets, advanced technologies like AI tools and machine learning can have limited impact. We're somewhat gazing into a crystal ball when we try to imagine how new technologies might drive improvements in rare disease diagnosis and drug discovery, but advances in AI and gene therapies, for example, will accelerate the pace of drug development, leading to treatments that will be more highly targeted and easier to deliver.
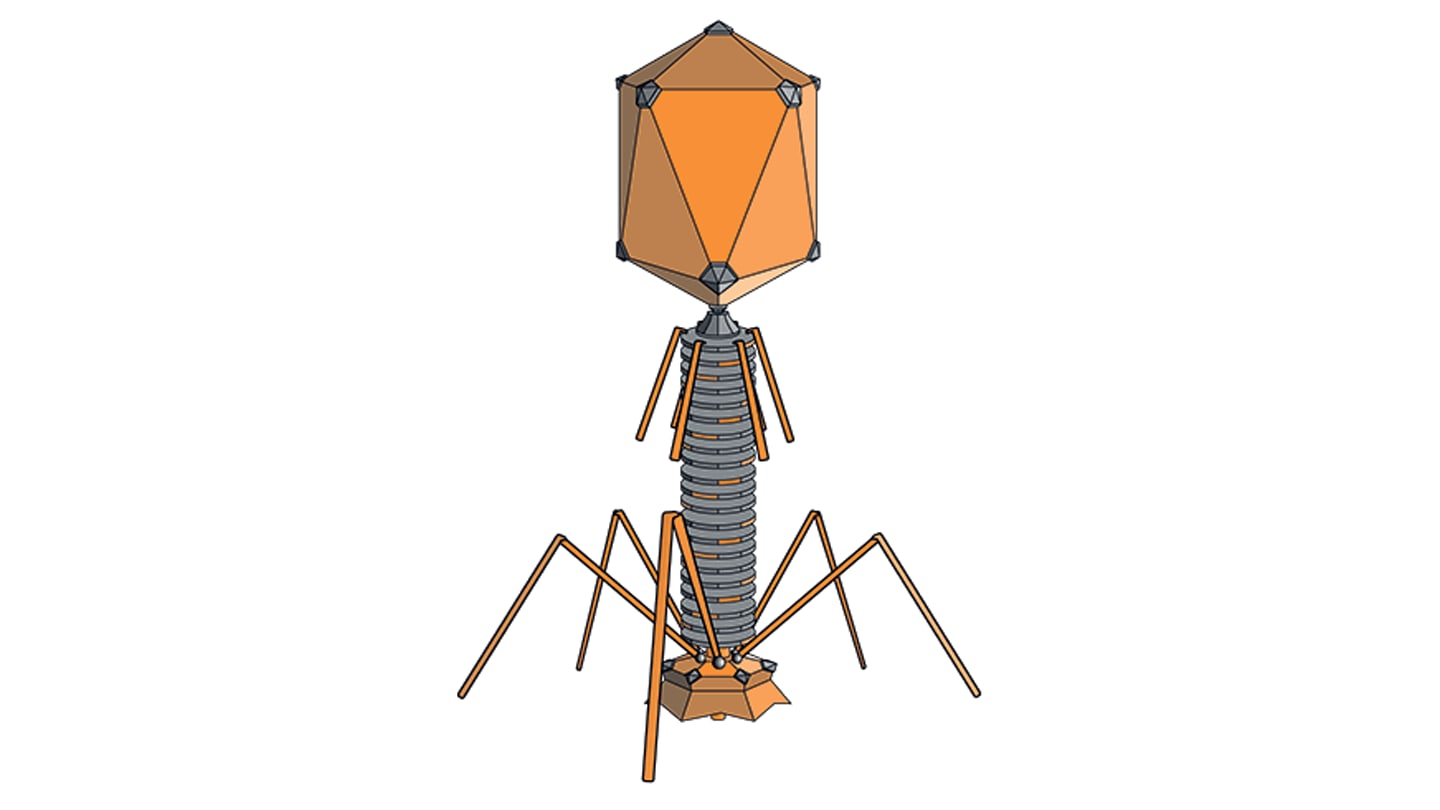
Already, technologies like gene editing and gene silencing allow scientists to develop highly targeted treatments, which is especially helpful for rare diseases, around 80 percent of which are monogenic – caused by a single-gene mutation. By focusing on fixing or replacing faulty genes, or silencing them, these drugs are working at the very deepest levels of biology – in the cell itself. We are well into the era of AI-designed drugs, which could transform not just the business case for rare disease drug development, but the lives of patients and their families.
While there remain obstacles to overcome, the applications of AI for genomic analysis, decision-support systems, image analysis, and much more, create the hope that rare disease diagnosis, which today remains a critical problem, will become much more rapid.
Showing symptoms
One of the most promising applications of AI in this field lies in its capacity to distinguish rare disease symptoms from those of more common conditions. Many rare diseases cause symptoms, such as fatigue, pain, or developmental delays, that are non-specific. Without access to specialist knowledge, these symptoms can be easily misattributed. A key factor is learning from real-world data. In a typical consultation, it may be near-impossible to research historical records to look for patterns, tell-tale signs, and other data-based clues – precisely what AI tools can do. If properly trained, these tools can detect and analyze symptom clusters that may elude even the most experienced doctors.
Early identification is at the very heart of the rare disease challenge. Improving it could be transformative. Faster diagnosis not only spares patients and families years of uncertainty and emotional distress, it also opens the door to earlier interventions, better management, and in some cases, lifesaving treatments. In pediatric cases especially, identifying a rare disease early can prevent irreversible damage during the critical developmental months and years.
“Gene silencing” is rapidly becoming a powerful tool for targeting mutated genes, stopping them from producing toxic proteins, and AI can rapidly analyze vast datasets to identify potential drug targets and predict how they might work. It can also help design key gene silencing technologies, such as antisense oligonucleotides (ASOs), and small interfering RNAs (siRNAs). Designing an ASO to target a single-gene mutation is a far more tractable problem.
Seeking approval
The expense, effort, and time taken to bring a drug to market is mind-blowing, and of course it may never make it - indeed, most don’t. From an analysis by PatentPC, only 12 percent of drugs that enter clinical trials eventually receive FDA approval. According to the same analysis, the average cost of developing a new prescription drug is approximately $2.6 billion – and it takes between 10 and 15 years from discovery to market approval. This is bad, but it gets worse. The agencies that underpin the entire process are hugely expensive themselves. The cost of regulatory compliance adds 15-25 percent to total drug development expenses, and the cost of a failed drug candidate can exceed $1 billion – again, according the PatentPC analysis.
By comparison with prescription drugs, the cost of bringing a rare disease drug (orphan drug) to market is typically between $1 billion and $2 billion. These drugs address, by definition, a limited market. However, government initiatives, starting with the Orphan Drug Act in the US in 1980, have created a more attractive regime for orphan drug development that includes financial incentives such as market exclusivity, tax credits, and fast-track approvals. That being said, it’s still an enormous financial gamble.
Structurally, it has been the smaller biotechs, on whom these huge financial burdens weigh most heavily, that have emerged as the primary source of rare disease drug research and development. As noted, somewhere between 80 and 85 percent of rare diseases are monogenic, making them better candidates for AI-designed drugs as there is a single protein that can be targeted. However, many diseases involve incredibly complex biological processes – with no easily identifiable, single protein to target. And there are further challenges;the same drug can affect individuals differently, due to genetic and biological variation. An AI-designed drug would need to account for every possible patient response, which may prove to be an insurmountable barrier – at least until we know more about the underlying biology and have sufficiently powerful tools.
AI – already incredible
Before AI, drug discovery was a hugely time-consuming process, subject to trial-and-error experiments and testing. The promise held out by advocates of advanced technology is that, not today, or tomorrow, but some day relatively soon, the accumulation of breakthroughs in multiple disciplines and technologies, for example quantum computing and AI, will combine to give us the ability to design drugs in a fraction of the current time.
Five years ago the first drug designed by AI reached clinical trials. It was the result of a collaboration between British startup Exscientia and a Japanese pharma, Sumitomo Pharma, who said the use of AI meant their drug got to clinical trials five times quicker than usual. So, there are already major breakthroughs that signal the future direction such technologies will deliver.
AI’s ability to find patterns in data means major improvements in the speed and accuracy of drug discovery. It can identify targets, discover potential treatments, and even design the molecular structure of potential drugs. According to a paper from June last year, in the National Library of Medicine, “AI models can predict how well a drug will bind to its target, forecast the efficacy and toxicity of drug compounds, or suggest new applications for old drugs.”
Large parts of the traditional drug discovery process can now be supplanted by tools that obviate the need for trial and error – which is an extraordinary leap forwards. Given the timescales and costs described above, this is genuinely game-changing. In a related area, last year’s Nobel Prize in Chemistry was awarded to Google’s AlphaFold, an AI tool that predicts the 3D structure of proteins from amino acid sequences – another example of how AI can improve the medicine discovery process, and another stepping stone on the path to the ultimate dream.
Google DeepMind spin-out Isomorphic Labs claims its AI models reduce the need for time-consuming experimental lab work. Its AI drug design system allows researchers to predict the way molecules will interact with, and bind to, proteins - and behave in the body. In January this year, the company said it plans to have drugs in clinical trials by the end of the year.
To cap it all, the first AI-discovered drug development was achieved by Insilico. Its drug for idiopathic pulmonary fibrosis is the first where both the target and compound were discovered using generative AI. The whole process took just 18 months. According to an analysis by ScienceDirect, between 2015 and 2024, 75 AI-developed drugs entered clinical trials, with the number under investigation increasing exponentially each year. And it seems to be working. According to an analysis published in the National Library of Medicine, AI-discovered molecules show a substantially high success rate (80-90 percent) in phase I clinical trials. Insilico’s drug, mentioned above, entered phase II clinical trials in the US and China in mid-2023 – yet another major milestone. The ScienceDirect report continues, “It seems like it’s only a matter of time before the first AI-invented medicines are treating patients.”
If proof were needed, investment in AI in the life sciences sector is booming; last year, McKinsey estimated that generative AI could create $28 to $53 billion a year in value through research, discovery, and clinical development activities.
In confidence
From a governance and ethical perspective, rapid innovation must be balanced with patient safety and privacy. New diagnostic tools or treatments powered by AI need rigorous oversight, particularly when using sensitive patient data. Mistakes and data breaches can erode public trust and impose slow adoption. AI is dramatically improving the efficiency and success rates of drug discovery, with many AI-discovered drugs entering clinical trials, and the first AI-designed medicines poised to reach patients soon. AI's ability to identify drug candidates, by analyzing vast amounts of complex data, is increasingly speeding up the process.
One day, at the push of a button, and near instantaneously, an AI tool will design a drug that combats any condition, taking into account known toxicity, safety, and side effects – factoring in patients’ genetic make-up, medical history and more. With that vision (or dream) firmly in mind, the process then becomes identifying the steps, the building blocks, that need to be put in place to achieve it – but that’s precisely where a strong focus on specific, smaller, goals, can do so much. And it’s precisely what we’re seeing with the breakthroughs listed above.
Technological innovation, used effectively in the life sciences, continues to drive improvements in productivity and in people’s lives. For the patients that need them, that’s where the real magic happens. Yes, there are issues and challenges – not least around patient confidentiality. But the promise is so great that we must ensure these are addressed such that the dream becomes extraordinary reality.